Hemorrhoids develop when the cluster of veins in the rectum or anus swell and stretch.
While they can be recurrent, painful, and embarrassing, they are rarely dangerous. This condition is also linked to constipation and excessive straining during defecation and becomes extremely common with age[1].
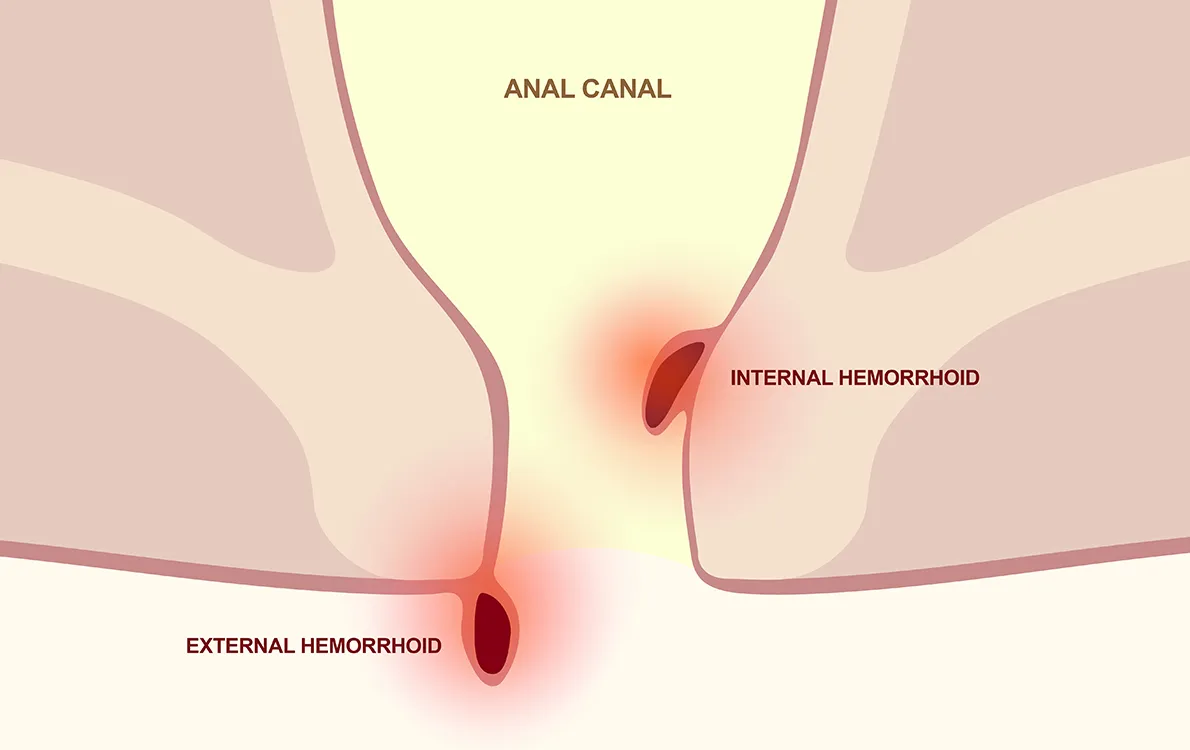
What’s the difference between internal and external hemorrhoids?
There are two types of hemorrhoids, categorized by their location. Internal hemorrhoids occur in the lower rectum, the terminal section of the large intestine and are usually painless.
External hemorrhoids form under the skin around the anus, causing irritation and damage to the skin. If a blood clot begins forming inside this type of hemorrhoid, it can cause significant pain. Fortunately, the clot typically dissolves and leaves behind a flap of excess skin.
Common symptoms of hemorrhoids
When this condition is symptomatic, it may cause[2]:
- Bleeding
- Pain
- Anal protrusion
- Itching
Classifying internal hemorrhoids
Internal hemorrhoids are further graded based on their appearance and the degree of prolapse[2]. Prolapse is a medical term to describe when internal organs like the blood vessels beneath the anus, push out of their usual position. These grades, known as Goligher’s classification help determine the severity of the hemorrhoid.
- Grade I: Internal bleeding but no prolapse
- Grade II: Prolapse only occurs during straining, but goes away on its own
- Grade III: Prolapse occurs during straining but requires it to be manual placed back into position
- Grade IV: The blood vessels beneath the anus always remain prolapsed
How common are hemorrhoids?
Since most hemorrhoids don’t cause symptoms, it is difficult to estimate how common this condition may be. One study of patients undergoing routine cancer screening found that 39 percent had hemorrhoids, and more than half did not report any symptoms[3]. In addition, hemorrhoids are more likely to develop in people between the ages of 45 to 65[3].
What causes hemorrhoids?
It isn’t clear what causes hemorrhoids but there are many well-known risk factors that increase the chance of developing them.
The strongest of these risk factors includel [4]:
- Straining and constipation: Adds excess pressure on the veins in the anus and rectum, which may cause them to stretch and swell.
- Obesity: This is often associated with a low-fiber diet and other gastrointestinal issues.
- Pregnancy[5]: More than one in four women will experience hemorrhoids during pregnancy due to extra abdominal pressure and hormonal changes.
- Chronic diarrhea[6]: This can cause inflammation in the anus or rectum.
- Low-fiber diet[6]: This can lead to straining and constipation.
You may be able to prevent hemorrhoids through maintenance of your gut health. This includes eating a healthy diet filled with fiber, drinking more water, and treating any potential constipation or diarrhea[7]. Staying active through exercise and avoiding having to sit for extended periods of time can also help[7].
When should I see a doctor?
If you regularly notice blood in your stool, prolapse, itching, or pain, it might be time to check in with your doctor. The doctor may perform a physical examination of the anus and rectum to look for signs of hemorrhoids or prolapse[4]. In addition to suggesting lifestyle changes and treatments, this initial appointment can rule out more severe conditions like colorectal cancer[4].
Treating hemorrhoids
The initial treatment of hemorrhoids involves lifestyle changes including:
- Eating more fiber: A diet containing at least 25 grams of fiber will promote healthy bowel movements and prevent constipation. If this is not possible through diet, over-the-counter fiber supplements can increase intake.
- Drinking more water: This will help make stools easier to pass and prevent excess straining and constipation.
- Stool softeners: This will also make stools easier to pass and prevent straining.
- Warm water bath[4]: Also called a sitz bath, submerging the butt and hips in warm water for 20 minutes after bowel movements, and two or three additional times per day can help reduce irritation and soothe pain and swelling.
There are also many over-the-counter remedies that provide temporary relief. These preparations often include two or more of the following[1],[4],[8]:
- Astringents (witch hazel): Protect irritated areas and relieve sense of discomfort or burning.
- Protectants (zinc oxide): Protect the skin and irritated areas to prevent dryness and provide soothing relief.
- Decongestants (phenylephrine): Shrinks blood vessels to relieve burning and swelling.
- Steroids: Lower swelling, redness, and itching.
- Topical anesthetics: Provided targeted pain relief.
- Flavonoids (diosmin for example Hemovel®): These bioactive compounds are used to reduce the pain, swelling and bleeding that come with hemorrhoids.
Conclusion
Hemorrhoids are a common condition characterized by the stretching or swelling of blood vessels in the anus or rectum. While this condition is often asymptomatic, it sometimes causes pain, irritation, and bleeding in the stool.
A doctor can help rule out more serious conditions and help provide you with a strategy to manage hemorrhoids: eating more fiber, drinking more water, warm baths, and stool softeners. In addition, over-the-counter treatments can provide you with the relief you need.
Hemovel® is a registered trademark owned by Norwell Consumer Healthcare Inc.
These products may not be right for you. Always read and follow the label.
This article has been sponsored by Hemovel® a registered trademark owned by Norwell Consumer Healthcare Inc.
References:
- Lohsiriwat V. Hemorrhoids: From basic pathophysiology to clinical management. World Journal of Gastroenterology. 2012;18(17):2009. doi:10.3748/wjg.v18.i17.2009
- American Gastroenterological Association Medical Position statement: Diagnosis and treatment of hemorrhoids . Gastroenterology. 2004;126(5):1461-1462. doi:10.1053/j.gastro.2004.03.001
- Riss S, Weiser FA, Schwameis K, et al. The prevalence of hemorrhoids in adults. International Journal of Colorectal Disease. 2011;27(2):215-220. doi:10.1007/s00384-011-1316-3
- Mott, T., Latimer, K., & Edwards, C. (2018). Hemorrhoids: diagnosis and treatment options. American family physician, 97(3), 172-179.
- Staroselsky, A., Nava-Ocampo, A. A., Vohra, S., & Koren, G. (2008). Hemorrhoids in pregnancy. Canadian Family Physician, 54(2), 189-190.
- Jacobs D. Hemorrhoids. New England Journal of Medicine. 2014;371(10):944-951. doi:10.1056/nejmcp1204188
- Jacobs D. Hemorrhoids. New England Journal of Medicine. 2014;371(10):944-951. doi:10.1056/nejmcp1204188 Hemorrhoids. MyHealth.Alberta.ca Government of Alberta Personal Health Portal. [4]. Accessed June 21, 2022.
- Hemorrhoid cream overview, uses and alternatives - goodrx. [4]. Accessed June 21, 2022.